The Conservative Draft Manifesto in 2010 said: "we will cut the cost of NHS administration by a third". This, apparently, was to be done by cutting management by 45%.
The Nuffield Trust have just released some slides showing how the NHS has changed since 2010 and what Lansley's new NHS will be like. I have extracted just the charts showing the organisations:
You can make the image bigger by clicking on it, but before you do that, have a look at the shapes out of focus. The left side has four types of organisations top to bottom; the right hand side has five (or six) types. Top to bottom are the layers of management. Lansley claimed to cut the layers of management, but he has clearly added to them. Further, if you look at the total number of organisations, the left side shows fewer separate organisations and the transition to the right shows more types of organisations: the system is getting more complicated. Bureaucracy comes from complication and Lansley's NHS is more complicated.
Thursday, 26 July 2012
Sunday, 8 July 2012
Self referral
"I haven't seen you for years, your condition must be bad: I only get to see the difficult cases."
This is what the consultant eye surgeon said to me at an emergency appointment at the eye clinic early in the summer of 2005. He was right, the last time I had appointment with him was seven years before. When I moved to the area I was referred to the hospital for diabetic retinopathy by my previous doctor. Retinopathy is a condition where the blood vessels on the retina grow large and weak and are liable to burst. Previously I had had a big bleed in one eye and had started a series of laser treatment. This treatment continued under the new consultant, having many thousands of laser burns per eye (a session every 3 months, then 6 months over a period of 5 years). I was referred to the eye surgeon's clinic and initially it was him that treated me, then when my eyes stablised another doctor from his team took over the treatment. In the follow up for my last treatment by the senior consultant he told me that there was one blood vessel that they could not treat and I should expect it to burst some time. Now I was in his office with the results of when that vessel bursting.
The previous few days I had removed about a tonne of hardcore from my garden. Over several years I had dug up stones and concrete in my garden and I wanted to get rid of this pile. I ordered a skip and spent a couple of days moving the hardcore from the pile to the skip. This involved a lot of bending down and picking up heavy stones. The next morning I noticed a strange mark on my retina and remembering the previous bleed, I went to my optician. He looked at my retina and told me to go immediately to the hospital eye clinic. I was fitted onto the list of one of the doctors and, after seeing my eye, he made an appointment the following week for the senior eye surgeon. And that is when he made the comment above.
The seriousness of the bleed made me a priority. Indeed, the bleed was so large that the surgeon called in two of the other doctors in the clinic to see the extent of the bleed and compare it to the photos of the vessel that had burst. There was an impromptu case meeting. The surgeon told me that I would need an operation under general anaesthetic where the gel in my eye (the vitreous humour) would be removed and then he would stop the bleeding of the vessel and clean up my retina. My eye would then be re-filled with an oil-like substance which my body would eventually absorb (over a period of about a month) and replace with more of the vitreous humour. The size of my bleed made me a priority for surgery and the surgeon's list was changed accordingly.
The surgery was successful, and the surgeon was able to clean up some of the damage from the previous bleed, so I had eyesight that was better than it had been for a decade. There is still some permanent damage and this is like having several blind spots in my eye. After the surgery I had a follow up with the eye surgeon and although I have had several follow up appointments for my retinopathy, I didn't see him again until I needed cataract surgery, which he also carried out.
The government has decided that in the interests of "patient choice" we all must have the choice of the "consultant-led team" for our care. This is an attempt to get closer to the US system of patient referrals. Self referrals are one of the causes of the high costs of the US system. If an American colleague gets a rash they will go and see "their" dermatologist. If I get a rash I will see my GP and if my GP thinks the rash needs the opinion of someone more specialist, I will be referred to the consultant dermatologist. The NHS system ensures that you get care according to need. It is the GP who decides what that need is: can they deal with it, or does it need a specialist. This is NHS prioritising, which some people call "rationing", but it is rationing only in the sense that GPs "ration" the work of the specialists to only those who need it. I have had countless arguments with American colleagues who interpret NHS prioritising as a form of denial of care. It isn't. The NHS ideal is that we get the care prioritised according to our clinical need. Those who do not get the care, do not need it.
Diabetic retinopathy cannot be "cured", so I still have 6 monthly monitoring of my retinas. If I was given the choice of consultant I would choose the eye surgeon who had operated on my eyes. I like his manner and how he explains my condition to me. But I also know that he is considered the best eye surgeon in the region. When it comes to their health, everyone wants the best. Every surgeon's time is limited, so he limits his time to the more serious conditions. My eyes are stable, so I will be a waste of his time and expertise. That is the way that the NHS works and it means that regardless of who you are or what you earn, if you need the expertise of the top clinician in the country, you will get it.
In the US the rationing of expertise is carried out through money: only those with the most amount of money can afford the best. In the NHS the "rationing" is carried out according to clinical need.
Lansley's plan of choice of "consultant-led team" will be a failure. The guidance says:
The 18 week referral to treatment waiting time target means that the more popular consultants (inevitably the most skilled) cannot handle the increased numbers of patients through longer waiting times. The only tool they have is the interpretation of the terms "consultant-led team" and "clinically appropriate". This policy will fail to give the patients the consultant they demand because responsible consultants will interpret "consultant-led team" to mean that they can delegate a patient to another doctor who is part of their team. They will also interpret "clinically appropriate" as I have outlined above: the consultant will see the higher priority cases and his junior staff will see the rest.
Lansley does not expect this policy to succeed because he knows that it cannot succeed. However, even as a failure this policy will achieve what Lansley wants: it will increase patient demand for self-referral, and that will lead us to a healthcare system that will be worse for us because we will not get the care we need, and it will lead to a system that most of us cannot afford.
This is what the consultant eye surgeon said to me at an emergency appointment at the eye clinic early in the summer of 2005. He was right, the last time I had appointment with him was seven years before. When I moved to the area I was referred to the hospital for diabetic retinopathy by my previous doctor. Retinopathy is a condition where the blood vessels on the retina grow large and weak and are liable to burst. Previously I had had a big bleed in one eye and had started a series of laser treatment. This treatment continued under the new consultant, having many thousands of laser burns per eye (a session every 3 months, then 6 months over a period of 5 years). I was referred to the eye surgeon's clinic and initially it was him that treated me, then when my eyes stablised another doctor from his team took over the treatment. In the follow up for my last treatment by the senior consultant he told me that there was one blood vessel that they could not treat and I should expect it to burst some time. Now I was in his office with the results of when that vessel bursting.
The previous few days I had removed about a tonne of hardcore from my garden. Over several years I had dug up stones and concrete in my garden and I wanted to get rid of this pile. I ordered a skip and spent a couple of days moving the hardcore from the pile to the skip. This involved a lot of bending down and picking up heavy stones. The next morning I noticed a strange mark on my retina and remembering the previous bleed, I went to my optician. He looked at my retina and told me to go immediately to the hospital eye clinic. I was fitted onto the list of one of the doctors and, after seeing my eye, he made an appointment the following week for the senior eye surgeon. And that is when he made the comment above.
The seriousness of the bleed made me a priority. Indeed, the bleed was so large that the surgeon called in two of the other doctors in the clinic to see the extent of the bleed and compare it to the photos of the vessel that had burst. There was an impromptu case meeting. The surgeon told me that I would need an operation under general anaesthetic where the gel in my eye (the vitreous humour) would be removed and then he would stop the bleeding of the vessel and clean up my retina. My eye would then be re-filled with an oil-like substance which my body would eventually absorb (over a period of about a month) and replace with more of the vitreous humour. The size of my bleed made me a priority for surgery and the surgeon's list was changed accordingly.
The surgery was successful, and the surgeon was able to clean up some of the damage from the previous bleed, so I had eyesight that was better than it had been for a decade. There is still some permanent damage and this is like having several blind spots in my eye. After the surgery I had a follow up with the eye surgeon and although I have had several follow up appointments for my retinopathy, I didn't see him again until I needed cataract surgery, which he also carried out.
The government has decided that in the interests of "patient choice" we all must have the choice of the "consultant-led team" for our care. This is an attempt to get closer to the US system of patient referrals. Self referrals are one of the causes of the high costs of the US system. If an American colleague gets a rash they will go and see "their" dermatologist. If I get a rash I will see my GP and if my GP thinks the rash needs the opinion of someone more specialist, I will be referred to the consultant dermatologist. The NHS system ensures that you get care according to need. It is the GP who decides what that need is: can they deal with it, or does it need a specialist. This is NHS prioritising, which some people call "rationing", but it is rationing only in the sense that GPs "ration" the work of the specialists to only those who need it. I have had countless arguments with American colleagues who interpret NHS prioritising as a form of denial of care. It isn't. The NHS ideal is that we get the care prioritised according to our clinical need. Those who do not get the care, do not need it.
Diabetic retinopathy cannot be "cured", so I still have 6 monthly monitoring of my retinas. If I was given the choice of consultant I would choose the eye surgeon who had operated on my eyes. I like his manner and how he explains my condition to me. But I also know that he is considered the best eye surgeon in the region. When it comes to their health, everyone wants the best. Every surgeon's time is limited, so he limits his time to the more serious conditions. My eyes are stable, so I will be a waste of his time and expertise. That is the way that the NHS works and it means that regardless of who you are or what you earn, if you need the expertise of the top clinician in the country, you will get it.
In the US the rationing of expertise is carried out through money: only those with the most amount of money can afford the best. In the NHS the "rationing" is carried out according to clinical need.
Lansley's plan of choice of "consultant-led team" will be a failure. The guidance says:
"Patients who want to should be able to choose a particular named consultant-led team for their first consultant-led outpatient appointment where it is clinically appropriate. The right to access services within maximum waiting times under the NHS Constitution continues and applies to patients who choose to be referred to a named consultant-led team."
The 18 week referral to treatment waiting time target means that the more popular consultants (inevitably the most skilled) cannot handle the increased numbers of patients through longer waiting times. The only tool they have is the interpretation of the terms "consultant-led team" and "clinically appropriate". This policy will fail to give the patients the consultant they demand because responsible consultants will interpret "consultant-led team" to mean that they can delegate a patient to another doctor who is part of their team. They will also interpret "clinically appropriate" as I have outlined above: the consultant will see the higher priority cases and his junior staff will see the rest.
Lansley does not expect this policy to succeed because he knows that it cannot succeed. However, even as a failure this policy will achieve what Lansley wants: it will increase patient demand for self-referral, and that will lead us to a healthcare system that will be worse for us because we will not get the care we need, and it will lead to a system that most of us cannot afford.
Wednesday, 4 July 2012
Circle Bath
This is an interesting presentation (pdf) by Circle aimed at their investors. I want to show two graphs from this presentation.
The first one shows vividly how the NHS is subsidising the debt ridden Circle Holdings. The red bars are the private patients and their figures are generally declining over the year. The black bars are the NHS patients and payment for these consistently provides much more income than the income from private patients. Without the NHS patients Circle would go bust; without Circle, the NHS would continue quite happily. Who needs who?
This second graph shows the "market share" between three hospitals in the Bath area, two private hospitals (including CircleBath) and the local NHS provider, the Royal United Hospital. The market share of the BMI hospital is broadly flat, and the small; peaks and troughs more or less correspond to the red bars on the previous graph (ie where the red bars are smaller and CircleBath have fewer private patients, there's an increase in BMI private patients). The interesting line is the decline of the market share of RUH which matches the rise of CircleBath.
How is CircleBath doing this? Well, it is not by being efficient and making a profit. Quite the opposite, they appear to be using their boutique hospital as a loss leader. The hospital had a revenue of £12.2m in 2011 (that is, the income of the hospital). Circle Holdings overall has a turnover of £75m on which it makes a loss of £14m. Circle's other hospital (in 2011) was the ISTC (Independent Sector Treatment Centre) at Nottingham which had a turnover of £51m on which it maked a profit of £2.4m. (Circle ran another clinic in Burton for the first 7 months of 2011, but this was a small unit, with an income of £1.5m). Considering Circle makes a profit at Nottingham on NHS work and it makes a loss over all, it is clear that the company makes a huge loss at CircleBath. Circle cannot make a profit from its private work, and any profits it makes from NHS work go to alleviate the losses they make from treating private patients.
The NHS "competitor" is RUH. This has an annual income of £216m, but the trust has a historic debt of £40m. The trust have been in surplus since 2007, and paying off this debt, and the current surplus is £4.2m. The trust has a loan from the Department of Health of £38m payable over 20 years, and like many of these loans it is at an eye popping rate of 5.05%. The government keeps boasting that they can borrow at historically low interest rates, so why are they lending this money at loanshark rates to NHS Trusts?
Clearly the situation in Bath is far from ideal. Circle are running a hospital at a loss poaching patients from the local NHS hospital. If CircleBath was an NHS hospital it would have been put into administration by now. Instead, it is allowed to threaten the viability of the local NHS trust by poaching patients and treating them for NHS rates that are less than they need to sustain the hospital.
The first one shows vividly how the NHS is subsidising the debt ridden Circle Holdings. The red bars are the private patients and their figures are generally declining over the year. The black bars are the NHS patients and payment for these consistently provides much more income than the income from private patients. Without the NHS patients Circle would go bust; without Circle, the NHS would continue quite happily. Who needs who?
This second graph shows the "market share" between three hospitals in the Bath area, two private hospitals (including CircleBath) and the local NHS provider, the Royal United Hospital. The market share of the BMI hospital is broadly flat, and the small; peaks and troughs more or less correspond to the red bars on the previous graph (ie where the red bars are smaller and CircleBath have fewer private patients, there's an increase in BMI private patients). The interesting line is the decline of the market share of RUH which matches the rise of CircleBath.
How is CircleBath doing this? Well, it is not by being efficient and making a profit. Quite the opposite, they appear to be using their boutique hospital as a loss leader. The hospital had a revenue of £12.2m in 2011 (that is, the income of the hospital). Circle Holdings overall has a turnover of £75m on which it makes a loss of £14m. Circle's other hospital (in 2011) was the ISTC (Independent Sector Treatment Centre) at Nottingham which had a turnover of £51m on which it maked a profit of £2.4m. (Circle ran another clinic in Burton for the first 7 months of 2011, but this was a small unit, with an income of £1.5m). Considering Circle makes a profit at Nottingham on NHS work and it makes a loss over all, it is clear that the company makes a huge loss at CircleBath. Circle cannot make a profit from its private work, and any profits it makes from NHS work go to alleviate the losses they make from treating private patients.
The NHS "competitor" is RUH. This has an annual income of £216m, but the trust has a historic debt of £40m. The trust have been in surplus since 2007, and paying off this debt, and the current surplus is £4.2m. The trust has a loan from the Department of Health of £38m payable over 20 years, and like many of these loans it is at an eye popping rate of 5.05%. The government keeps boasting that they can borrow at historically low interest rates, so why are they lending this money at loanshark rates to NHS Trusts?
Clearly the situation in Bath is far from ideal. Circle are running a hospital at a loss poaching patients from the local NHS hospital. If CircleBath was an NHS hospital it would have been put into administration by now. Instead, it is allowed to threaten the viability of the local NHS trust by poaching patients and treating them for NHS rates that are less than they need to sustain the hospital.
NHS funding
Today, the Nuffield Trust have published a report about NHS funding carried out by the IFS (pdf).
The IFS say that:
I have mentioned before, these three trends:
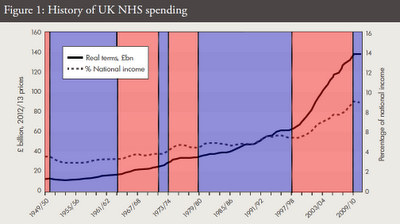
For my analysis I only had data (for England) from 1974, the IFS show data (for the UK) from 1949 to present. This data shows that the £1bn/yr real terms increase started at about 1960. I have copied their graph (Figure 1) and coloured it to show the government in power (blue is Conservative, red is Labour):
The IFS say that:
"Public spending on the UK NHS has increased faster than economy-wide inflation since the 1950s, with an average real growth rate of 4.0 per cent a year between 1949/50 and 2010/11"This is a silly statement because it is a wide date range, with some widely different government policies and it makes no sense to give an average. They may as well tell us that the average person has just under two legs, it has just as much meaning. Also, an average increase of 4% a year is a geometric increase (ie non-linear, the gradiet of the graph is not constant) whereas the actual data shows that the increases were broadly linear with three general trends.
I have mentioned before, these three trends:
- 1974 to 1998 there is a year-on-year increase in real terms of around £1bn each year
- 1998 to 2010 there has been a real terms increase of approximately £4.8bn every year
- 2010 to 2015 there is real terms flat funding
For my analysis I only had data (for England) from 1974, the IFS show data (for the UK) from 1949 to present. This data shows that the £1bn/yr real terms increase started at about 1960. I have copied their graph (Figure 1) and coloured it to show the government in power (blue is Conservative, red is Labour):
The Wilson/Callaghan Labour government suffered from the oil crisis and IFS imposed austerity, but it still increased NHS funding overall. The Thatcher/Major period also increased NHS funding. The Cameron period is clearly a new shift, and the IFS is suggesting that a Cameron government after 2015 may provide increases somewhere between flat funding and Thatcher levels of real terms increases.
Subscribe to:
Comments (Atom)